|
HEAVY PERIODS
Heavy menstrual bleeding (known as Menorrhagia) is a common disorder in women. Heavy periods are common, about one third of women seek treatment for it, but it is not normal. It is difficult to define exactly what a heavy period is because it varies among women. Most women will lose less than 16 teaspoons of blood (80ml) during their period, with the average being around 6 to 8 teaspoons. Most women have a good idea about how much bleeding is normal for them during their period and can tell when this changes. Heavy periods may be a sign of an underlying health problem that needs treatment. It can be caused by a number of conditions including problems with the uterus and hormones. Blood loss from heavy periods can lead to a condition called iron-deficiency anemia. Symptoms Your periods may be heavy if you:
PAINFUL PERIODS Pain associated with menstruation is called dysmenorrhea. There are two types of dysmenorrhea, primary and secondary. Primary dysmenorrhea is common menstrual cramps that are not due to disease. The pain usually begins 1 or 2 days before, or when menstrual bleeding starts, and is felt in the lower abdomen, back, or thighs. The pain can last for 1 to 3 days, and may be associated with nausea, vomiting, fatigue, and even diarrhea. It is usually caused by natural chemicals called prostaglandins that are made in the lining of the uterus. These cause the uterus to contract. As menstruation continues and the lining of the uterus is shed, the prostaglandin levels fall, and period pain decreases in severity. Secondary dysmenorrhea is less common and is caused by a disorder in the reproductive system. This type of pain often lasts longer than normal menstrual cramps. It may begin a few days before a menstrual period starts. The pain may get worse as the menstrual period continues and may even persist after it ends. CAUSES The following conditions may cause either Heavy Period bleeding or Painful periods (or both). Fibroids Fibroids are non-cancerous growths that develop in or around the uterus. Endometriosis Endometriosis is a condition where the tissue that lines the uterus (endometrium) is found outside the uterus, such as in the ovaries and fallopian tubes. Adenomyosis Adenomyosis is a condition where tissue from the uterus lining (endometrium) becomes implanted in the wall of the uterus. PID Pelvic inflammatory disease (PID) is an infection in the upper genital tract (the uterus, fallopian tubes or ovaries). It can cause symptoms like pelvic or abdominal pain, bleeding after sex or between periods, vaginal discharge and fever. IUD An IUD (intrauterine contraceptive device) can make your periods heavier for the first 3 to 6 months after insertion. The following conditions may also cause heavy bleeding. Irregular Ovulation If a woman does not ovulate regularly, areas of the lining of the uterus can become too thick. This condition is common during puberty and just before menopause. It also can occur in women with certain medical conditions, such as polycystic ovary syndrome (PCOS) and Hypothyroidism. Cancer Heavy menstrual bleeding can be an early sign of endometrial cancer. Most cases of endometrial cancer are diagnosed in women in their mid 60s who are past menopause. Anticoagulant Medication Blood thinners (such as aspirin, and other drugs) are taken to prevent blood clots. However, if the blood becomes too thin, there is an increased risk of bleeding, which may result in heavy menstrual bleed. Blood Clotting Disorders Persons who were born with conditions that prevent the blood from clotting properly (such as Von Willebrand Disease) are at risk of bleeding. Women with blood clotting disorders at risk for heavy menstrual bleed. DIAGNOSIS To determine the cause of heavy and/or painful periods, several tests may be done, some of which are mentioned below. Pelvic Exam, Pregnancy Test, Blood Test, Urine Test These may be done to identify Pelvic Inflammatory Disease, Pregnancy, Sexually Transmitted Infections, and other conditions. Ultrasound This will allow any abnormalities in your reproductive organs to be detected, such as fibroids. Hysteroscopy In this procedure, a thin, lighted scope is inserted into the vagina, through the cervix and into the uterus. It allows the inside of the uterus to be seen, and can identify abnormalities such as fibroids and polyps. Endometrial Biopsy and Dilatation & Curettage With Endometrial biopsy, a sample of the endometrium or lining of the uterus is removed and looked at under a microscope. A surgical procedure called dilation and curettage (D&C) is a similar test, where the lining of the uterus is scraped and then examined under the microscope. The endometrial tissue can then be examined for cancer or other abnormalities. Laparoscopy Laparoscopy is a surgical procedure, where small cuts are made in the abdomen through which a laparoscope is inserted. It can be used to look at the internal organs, as well as take samples of tissue for a biopsy. Laparoscopy is best for diagnosing Endometriosis. TREATMENT Both heavy periods and painful periods can be treated with NSAIDS and Hormonal birth control methods. NSAIDS Nonsteroidal anti-inflammatory drugs (NSAIDS), such as ibuprofen, can help to control heavy bleeding and relieve menstrual cramps. Hormonal Birth Control Methods Birth control methods that contain estrogen and progestin, such as the pill, the patch, and the vaginal ring, can make periods more regular and reduce bleeding. They are also good at relieving severe period pain. Heavy periods can also be treated using the methods below. Tranexamic acid This is a prescription medication that treats heavy menstrual bleeding. It is a tablet that is taken each month at the start of the menstrual period. Dilation and Curettage (D&C) This procedure can be done to reduce menstrual bleeding by removing the top layer of the uterus lining. Endometrial Ablation This procedure involves removing all or part of the lining of the uterus. It destroys the lining of the uterus, and thereby reduces menstrual bleeding. Surgery Myomectomy is surgery to remove fibroids without removing the uterus. Hysterectomy is the surgical removal of the uterus. Hysterectomy is used to treat fibroids, Adenomyosis and endometrial cancer. After the uterus is removed, a woman can no longer get pregnant and will no longer have periods. Tip#1: Exercise Staying active during your period may help to reduce pain. Try gentle exercises such as walking, cycling or swimming. Tip#2: Heat and Massage Putting a heat pad or hot water bottle (wrapped in a towel) on your abdomen may help reduce pain. Light, circular massage around your lower abdomen may also help to reduce pain. Tip#3: TENS Transcutaneous Electronic Nerve Stimulation (TENS) is a small battery-operated device that delivers a mild electrical current to your abdomen, which can help to reduce pain. Tip#4: Alternative Medicine Vitamin B1 or magnesium supplements may help to reduce period pain and bloating. Acupuncture may also be helpful in relieving menstrual pain in some persons. Tip#5: Hormonal Birth Control If you are using hormonal birth control to relieve heavy bleeding or severe menstrual pain, remember to be consistent. These methods are less effective if they are not used correctly (or regularly). Tip#6: Vaginal bleeding after menopause Any woman, who has reached menopause, that has started having “period-like” vaginal bleeding again should see their doctor as soon as possible, to rule out endometrial cancer. Tip#7: Fertility When choosing a surgical method to treat heavy periods, be mindful of those treatments that may prevent you from having children in the future, such as Endometrial ablation and Hysterectomy. I hope these tips on HEAVY and PAINFUL periods were helpful; Remember, Your Health Is Invaluable! By Dr. J. Lawarna Matthew Acknowledgements Cleveland Clinic https://my.clevelandclinic.org/health/diseases/17734-menorrhagia-heavy-menstrual-bleeding The American College of Obstetrician and Gynecology https://www.acog.org/Patients/FAQs/Heavy-Menstrual-Bleeding https://www.acog.org/Patients/FAQs/Dysmenorrhea-Painful-Periods visit the links above for more information
0 Comments
Depression, particularly Major Depressive Disorder (or clinical depression), is a common but serious mood disorder. Most people go through periods of feeling down, but when a person is depressed, they feel persistently sad for weeks or months, rather than just a few days. Depression causes feelings of sadness, a loss of interest in activities once enjoyed and many other symptoms. Depression may become a serious health condition; it can cause the affected person to suffer significantly, and function poorly at work, school and in the family. At its worst, depression can lead to suicide. It is a genuine health condition, a real illness with real symptoms. Depression isn't something that someone can just "snap out of" by "pulling him or herself together". There are other forms of depression, which are slightly different to Major Depressive Disorder. Some of these include Persistent depressive disorder (also called dysthymia), Postpartum depression, Psychotic depression and Bipolar Disorder. Depression may start gradually, so it can be difficult to notice it at first. Many people try to cope with their symptoms of depression without recognizing that they are affected. Sometimes it may take a friend or family member to notice that something is wrong or different about the person. Depression can be mild, moderate or severe; mild to moderate depression has some/ significant impact on a person’s life. With severe depression however, it can sometimes be impossible for someone to get through daily life. Grief/ Sadness and Depression Some persons have experienced difficulties in life such as the death of a loved one, the loss of a job or the ending of a relationship. It is normal for feelings of sadness or grief to develop in response to these situations. Grief shares some of the same features of depression. Both grief and depression may involve intense sadness and withdrawal from usual activities, however they are different in many ways. For example in grief, self-esteem is usually maintained, but in major depressive disorder, feelings of worthlessness are common. WHO Key facts
RISK FACTORS Depression is caused by a combination of genetic, biological, environmental, and psychological factors. There may be many causes (and triggers), only a few are mentioned below.
SYMPTOMS In general persons who are depressed feel sad, hopeless and lose interest in things they used to enjoy. Symptoms must last at least two weeks for a diagnosis to be made. Not everyone who is depressed experiences every symptom; some people experience only a few symptoms while others may experience many. Psychological Symptoms
Physical Symptoms
Social Symptoms
TREATMENT Depression can be treated; the earlier treatment begins, the more effective it is. It is usually treated with medications, psychotherapy, or a combination of both. Medication (Antidepressants) 1) Antidepressants are medicines that treat the symptoms of depression. Most persons with moderate or severe depression benefit from antidepressants, (however, not everyone does). The benefits of these medicines may not be seen for up to two months. It is important to give antidepressants adequate time to work before concluding that they are not effective. If a patient feels little or no improvement after several weeks, then the dose of the medication can be adjusted, another medication can be added or a new antidepressant may be recommended. 2) Most doctors advise patients to keep taking antidepressants for 6 to 12 months after they no longer feel depressed; after that time, the doctor will help you slowly and safely decrease the dose. Do not stop taking antidepressants without the help of a doctor. Persons, who stop taking antidepressants immediately after they feel better, are at risk of the depression returning. Stopping them abruptly can also cause withdrawal symptoms, (flu-like symptoms, anxiety, dizziness, vivid dreams at night, sensations in the body that feel like electric shocks). 3) Antidepressants such as SSRIs (Selective Serotonin Reuptake Inhibitors), Serotonin-Noradrenaline Reuptake Inhibitors (SNRIs), and Tricyclic antidepressants (TCAs), help to increase the level of serotonin and noradrenaline in the brain, which are considered to be ”good mood” chemicals. Examples include:
4) Antidepressants generally have side effects; these should improve within a few weeks, although some may persist for much longer. They include
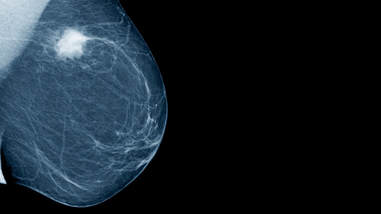
Psychotherapy Psychotherapy or “talk therapy,” may be used alone for treatment of mild depression. For moderate to severe depression, psychotherapy is often used along with antidepressant medications. Cognitive behavioral therapy (CBT) has been found to be effective in treating depression. Depending on the severity of the depression, treatment can take a few weeks or much longer. Electroconvulsive Therapy (ECT) This is a medical treatment most commonly used for persons with severe major depression who have not responded to other treatments. During ECT, a carefully calculated electric current is passed to the brain through electrodes placed on the head. This procedure helps relieve the symptoms of depression. The link below has FAQs and more information on ECT. https://www.rcpsych.ac.uk/mentalhealthinformation/therapies/electroconvulsivetherapy,ect.aspx Tip#1: Diet and Exercise Exercise is known to improve the mood. Ensure that you are regularly active; this can help to create positive feelings. Also ensure a healthy diet, and avoid alcohol and tobacco. Tip#2: Sleep Some persons with depression suffer from insomnia or over sleeping. It is important to achieve a balance; try to get an adequate amount of sleep every night. (Ensure a healthy sleep environment also.) Tip#3: Socialize Do not consistently isolate yourself; try to occasionally spend time with other people. Also you can confide in a trusted friend or relative about your illness and/or how you are coping. Research shows that ‘talking’ can help people recover from depression and cope better with stress. Tip#4: Be Patient Expect your mood to recover gradually, not immediately. Also, remember to give psychotherapy and antidepressants a few weeks before you notice an improvement in symptoms. (Tell you doctor of any side effects.) Tip#5: Taking Care of someone with Depression Caring for someone with depression may lead to a strained relationship between you and that person. Try finding a support group and/or talking to others in a similar situation; this might be very helpful. Also, if you are having relationship or marriage difficulties, because your partner is depressed, consider seeing a relationship counselor. They may be able to talk things through with both of you. Tip#6: Suicide The majority of suicide cases are linked to mental disorders, especially severe depression. Contact a health care provider as soon as possible if you are feeling suicidal, they will be able to assist you. If you see or know a friend or relative who show any warning signs of being suicidal, let them know that they are not alone and that you care about them. Offer them support and solutions to their problems, and get them professional help. Tip#7: Other Education Material Persons who are depressed should continue to educate themselves about this illness. Download this booklet using the link below, for more information on depression. https://www.nimh.nih.gov/health/publications/depression-what-you-need-to-know/depression-what-you-need-to-know-pdf_151827_151827.pdf I hope that these tips on DEPRESSION were helpful; Remember, Your Health Is Invaluable. By Dr. J. Lawarna Matthew Acknowledgements National Institute of Mental health (NIMH) American Psychiatric Association Visit https://www.nimh.nih.gov/health/topics/depression/index.shtml#part_145399 and https://www.psychiatry.org/patients-families/depression/what-is-depression for more information. Breast cancer starts when abnormal cells in the breast begin to grow uncontrollably. These cells usually form a tumor that can often be seen on an x-ray or felt as a lump. It is spread when the cancer cells get into the blood or lymph system and are carried to other parts of the body. Breast cancer occurs almost entirely in women, but men can get it too.
Breast cancers can start from different parts of the breast. Most of them begin in the ducts that carry milk to the nipple (ductal cancers). Some start in the glands that make the breast milk (lobular cancers). There are several other types of breast cancers that are less common, including inflammatory breast cancer and Paget's disease of the breast. According to the WHO, breast cancer is the most common cancer among women. It affects around 2.1 million women each year, and also causes the greatest number of cancer-related deaths among women. In 2018, it is estimated that 627,000 women died from breast cancer – that is approximately 15% of all cancer deaths among women. CAUSES/ RISK FACTORS Changes or mutations in DNA can cause normal breast cells to become cancer. Persons can inherit these DNA mutations or abnormal genes from their parents. Women who have a BRCA1 mutation or BRCA2 mutation (or both) have a significantly higher risk of being diagnosed with breast cancer. Other lifestyle-related risk factors, such as diet and physical activity, may affect a person’s chance of developing breast cancer. Hormones, especially estrogen, seem to play a role in many cases of breast cancer as well. Some of the common risk factors for breast cancer include:
II. Older age at first birth or never having given birth III. Starting menopause at a later age
SYMPTOMS The most common symptom of breast cancer is a new lump or mass in the breast. The lump may be hard or soft, painless or painful. Not all breast lumps are cancer; it is important to get all new breast masses, lumps or other changes investigated by a doctor as soon as possible. Other possible symptoms of breast cancer include:
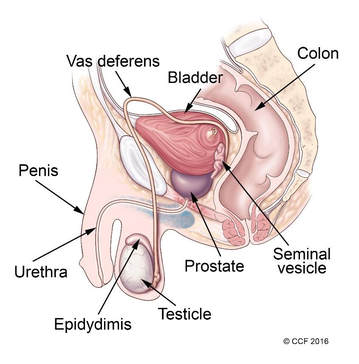
DIAGNOSIS There are several ways to identify and investigate a breast lump. These include breast exams, mammograms, ultrasound and biopsy. Screening Screening consists of testing women to identify cancers before any symptoms develop. Various methods have been evaluated as breast cancer screening tools, including breast self-exam, clinical breast exam and mammography. Breast Self-Exam Adult women should do breast self-exams at least once a month; this allows lumps to be detected early. Many women, who were diagnosed with breast cancer, detected their own breast lump. Women should be familiar with how their breasts normally look and feel so that they could notice changes easily. For more information on how to do breast self-exams visit the link below. https://www.nationalbreastcancer.org/breast-self-exam Clinical Breast Exam This is an examination of both breasts performed by a trained health professional. They are similar to breast self-exam, and the lymph nodes under the arms are examined more thoroughly. If a lump were found, additional tests would need to be done such as a mammogram or ultrasound. Mammography and Ultrasound A mammogram uses low-energy X-rays to identify abnormalities in the breast. Mammograms can show a breast lump before it can be felt, which is why it is the test most preferably used to screen for breast cancer. Women should start having regular mammograms by the age of 50 years (or at 40 years old if you have a family history of breast cancer); this may be yearly, or every other year. A breast ultrasound is another imaging test that is done after finding a lump during a breast exam. Ultrasounds are also good at determining whether a breast lump is cystic or solid. If the lump is solid then a biopsy should be done. Biopsy A breast biopsy is usually done by using a needle to remove some of the cells from the lump in the breast. The cells are then observed by a pathologist under the microscope, to determine whether or not the lump is cancer. If the results prove that the lump is in fact cancerous, then a few more tests may be done to determine the best course of treatment. Breast Cancer Hormone Receptor Status (if cancer is diagnosed) Estrogen and Progesterone Receptor Test This is a laboratory test to measure the amount of estrogen and progesterone (hormone) receptors that are in the cancer tissue. If breast cancer cells have estrogen receptors, the cancer is called ER-positive breast cancer. If breast cancer cells have progesterone receptors, the cancer is called PR-positive breast cancer. Most breast cancers are ER and/or PR positive. These breast cancers usually grow more quickly, and may respond to treatment that blocks estrogen and progesterone, which stops the cancer from growing. HER2 Status (if cancer is diagnosed) Human Epidermal Growth Factor type 2 receptor (HER2 Test) HER2 is a gene that can be a factor in the development of breast cancer. This laboratory test measures how many HER2 genes there are in a sample of breast tissue. If there are more HER2 genes than normal, the cancer is called HER2 positive. HER2-positive breast cancers tend to grow faster and are more likely to spread and return, compared to HER2-negative breast cancers. These breast cancers can be treated with drugs that target the HER2 protein. TREATMENT Breast cancer is treated using a combination of surgery, radiotherapy, chemotherapy and hormone therapy. Surgery Surgery is the most common type of treatment for breast cancer. There are two types of surgery; the type a patient gets depends on the type of breast cancer, the size and location of the tumor and other factors. Mastectomy and Breast Conservation Surgery With a Mastectomy, the entire breast is removed, including some of the surrounding tissues. A double mastectomy involves the removal of both breasts. In Breast Conservation Surgery, only the part of the breast containing the cancer and some surrounding normal tissue is removed. Women who have had surgery for breast cancer also have the option of getting breast reconstruction surgery after. Radiotherapy Some women may need to have radiotherapy after surgery, to ensure that all remaining cancer cells are destroyed. Radiotherapy involves using high-energy rays; the type most commonly used is External Beam Radiation, where rays from a machine are aimed at the affected breast. There are other types of radiotherapy available. Radiotherapy may be done over several weeks and side effects may include skin reactions and pain in the breast or chest area. Chemotherapy Chemotherapy uses anti-cancer drugs that may be taken by mouth or given intravenously into the blood stream. Not all persons with breast cancer will need this treatment. Chemotherapy may be given before surgery to shrink large tumors, after surgery to try to kill any remaining cancer cells or it may be the main treatment used in persons with advanced cancer that has spread outside the breast. Hormone Therapy (and other treatment) Breast cancers that are ER-Positive or PR-Positive can be treated with hormone therapy after surgery, to prevent the cancer from coming back. These drugs block estrogen receptors, and thereby stop estrogen from stimulating breast cancer cells to grow. One such drug is Tamoxifen which can be taken for up to 5 years after surgery. Aromatase inhibitors (AIs) are another class of drugs commonly used by breast cancer patients; these drugs stop estrogen production. Herceptin is a drug commonly used to treat women with HER-2 positive breast cancers. Tip#1: Healthy Lifestyle Ensure you have a healthy diet, exercise regularly, maintain a healthy weight, and avoid tobacco use and excess alcohol consumption, because these habits are essential to reduce your risk of breast cancer. This is beneficial for all person affected by breast cancer as well. Tip#2: Breast Reconstruction Surgery If you think that you would want to have reconstructive surgery done, it is best to discuss this with your breast surgeon and a plastic surgeon before hand. This gives the surgical team time to plan out the best treatment options for you, whether you want to have the reconstructive surgery done immediately after your mastectomy or at a later date. Tip#3: Breastfeeding If you have the opportunity to breastfeed, take it. Breastfeeding may decrease your risk of getting breast cancer. There are also numerous benefits of it to the baby. Tip#4: Screening Adult women should perform regular breast exams, and should be familiar with their breasts enough, that they can detect subtle changes. Women 50 years or older should get regular mammograms, which can detect lumps not commonly felt. Tip#5: Living with breast cancer If you are living with breast cancer, visit the link below for more information. https://www.cancercenter.com/breast-cancer/living-with-breast-cancer/ I hope these tips on BREAST CANCER were helpful; remember Your Health Is Invaluable. By Dr. J. Lawarna Matthew Acknowledgements (National Institute of Health) National Cancer Institute American Cancer Society Breast Cancer Consortium-Archives (Image) Visit https://www.cancer.gov/types/breast and https://www.cancer.org/cancer/breast-cancer.html for more information The Prostate is a part of the male reproductive system, which includes the penis, prostate, and testicles. The prostate is located just below the bladder and in front of the rectum. It is about the size of a walnut and surrounds the urethra (the tube that empties urine from the bladder). Its function is to produce fluid that makes up semen. Cancer is a common term for a large group of diseases characterized by the growth of abnormal cells.
Prostate cancer is the second most commonly occurring cancer in men. There was an estimated recorded amount of 1.1 million cases and 307,000 deaths in 2012; the highest death rates of prostate cancer are found in African and Caribbean countries. Men of African decent have a significantly higher rate of prostate cancer than men of other races. It should be noted that black men:
RISK FACTORS
SYMPTOMS Symptoms of prostate cancer do not usually appear until the prostate is large enough to affect the urethra (the tube that carries urine from the bladder out of the penis). Some common symptoms include:
TESTS FOR PROSTATE CANCER The most commonly used tests to detect prostate cancer are blood tests, a physical examination of the prostate and a biopsy. Digital Rectal Exam (DRE) This used to be a very common test to screen for prostate cancer. For this test, a doctor would lubricate a gloved finger and gently insert it into the rectum. The prostate is just in front of the rectum, and if it is is enlarged or has an abnormal shape, then the doctor would easily notice it. The test is quick but might be uncomfortable. However this test as a method to screen for prostate cancer has been replaced by the PSA blood test. Blood Tests (PSA Testing/ Screening) This is a test that measures the level of Prostate Specific Antigen (PSA) in the blood, which is made by the prostate. A man’s PSA level may be raised if he has prostate cancer, and so the PSA test can be used as a prostate cancer-screening test. However, the test is not very specific, because PSA may be elevated in other circumstances too, (for example in some illnesses and when using some medications). Sometimes the PSA test can have false positive or false negative results. However, if a patient’s PSA level is abnormal, that is above the amount of 4.0 ng/mL, then a biopsy would have to be done in order to confirm whether a man has cancer or not. Biopsy A prostate biopsy is when a small piece of tissue is removed from the prostate (using a small needle) and looked at under a microscope to see if there are any cancer cells. It is the most accurate test to diagnose prostate cancer. If prostate cancer is diagnosed, other tests are done to find out if cancer cells have spread within the prostate or to other parts of the body. This process is called staging. The stage of prostate cancer determines the type of treatment. TREATMENT There are several possible treatments methods available for prostate cancer, these include:
Watchful waiting/ Active Surveillance Watchful waiting /Active surveillance is more of an observational approach to the disease. It involves having regular PSA tests, MRI scans and sometimes biopsies to ensure that any signs of advancement of the cancer are found as early as possible. This type of treatment is often recommended:
Surgery Surgery is a common treatment method to try to cure prostate cancer (if it has not spread outside the prostate gland). The main type of surgery for prostate cancer is a radical prostatectomy. In this operation, the surgeon removes the entire prostate gland plus some of the tissue around it. There are some common (serious) side effects of prostate surgery. These include:
Radiotherapy Radiotherapy involves using radiation or high-energy-rays to kill cancerous cells. In External Beam Radiation Therapy (EBRT), beams of radiation are focused on the prostate gland from a machine outside the body. This type of radiation can be used to try to cure earlier stage cancers. There are several other types of radiotherapy treatments available as well. Some side effects of radiotherapy include urinary problems, bowel problems and erectile dysfunction. Tip#1: Symptoms It is important to recognize prostate cancer early. Older men who begin noticing problems with urination, blood in the urine or semen and other symptoms should see a doctor as soon as possible. All men over 50 years, should ask their doctor to be screened using the PSA test, because cancer that is treated at an earlier stage leads to a better outcome. Tip#2: Diet A healthy diet may decrease the chance of developing prostate cancer. A plant-based diet is best and try to avoid processed foods. Also, avoid tobacco smoking and reduce alcohol consumption as much as possible. Tip#3: Exercise Regular physical activity has many benefits. It is said that regular exercise can help the body to fight cancer cells. Exercise also helps to maintain a healthy body weight. Everyone should aim for at least 150 minutes of moderate intensity exercise spread over 3 to 5 days per week. Tip#4: Active Surveillance If you and your doctor have agreed to use active surveillance as a treatment method for prostate cancer, then it is important to keep your doctor appointments and get your tests done on time. This will ensure that the cancer is being monitored appropriately. Tip#5: Surgery If you have agreed to have surgery done as a treatment for prostate cancer, you must be aware of the risks involved, including Infertility. This is important for younger men who may still want to start a family. If infertility is a concern for you, you might want to consider “banking” your sperm before the surgery. I hope these tips on PROSTATE CANCER were helpful; Remember your health is Invaluable. By Dr. J. Lawarna Matthew Acknowledgements American Cancer Society Center for Disease Control (CDC) American Urological Association Visit https://www.cdc.gov/cancer/prostate/basic_info/ and http://www.urologyhealth.org/urologic-conditions/prostate-cancer for more information. |
AuthorDr. J. Lawarna Matthew Archives
January 2021
Categories |
 RSS Feed
RSS Feed
